ORAL AND DENTAL DIAGNOSIS
THE NEED FOR IMPROVED STANDARDS OF COMMONLY USED EQUIPMENT FOR RECORDING OF EMG AND TMJ SOUNDS IN DENTAL CLINICS
DOI: https://doi.org/10.25241/stomaeduj.2023.10(1-4).art.1
Sven Erik Widmalm1
DDS, Odont, PhD
Professor Email: sew@umich.edu
*Corresponding author: Prof. Em. Sven Erik Widmalm, DDS, Odont, PhD.
Computer Science and Engineering Division, College of Engineering, University of Michigan, Ann Arbor, MI 48109, USA. Tel./Fax: +1 734-764-2390; e-mail: sew@umich.edu.
1 Computer Science and Engineering Division, College of Engineering, University of Michigan, Ann Arbor, MI 48109, USA
aDDS, Odont, PhD, Professor Emeritus; e-mail: sew@umich.edu; ORCIDiD:
https://orcid.org/0000-0002-6793-3011
Abstract
Recording both Electromyographic (EMG) and temporo-mandibular joint (TMJ) sounds using surface (SEMG) and intramuscular electrodes can prove to be extremely beneficial for both dental research and clinics. SEMG can provide a comprehensive overview, while needle EMG can be used to analyze the functioning of a specific muscle or muscle component. Amplifiers should have various power level options and a flat frequency response. When using needle electrodes for EMG recording, it is crucial to have a sampling rate of at least 10,000 Hz to capture the necessary waveforms.
Keywords: EMG; Evidence-Based Dentistry; Oral Diagnosis; TMJ; TMJ sounds;
1. EMG ANALYSIS
There are many applications where integration of EMG may be useful [1]. The early users of EMG were enthusiastic about the main virtue of integrated outputs as having the convenience of a numerical read-out, and that the output could be fed directly to automatic devices [2]. It was, however, soon realized that integration also had dangers. Grossman and Weiner published 1966 [3] about those hazards, such as failure to discriminate between artifacts and unit potentials, where naked-eye examination of standard records is superior. Basmajian pointed out [2] that one can only compare the levels of the integrated curve with parts of the same curve”.
1.1. Settings
It is desirable to have options for different settings of gain, sampling rate, bandwidth, and frequency response. Amplitude, waveform, and contraction pattern as seen in the raw EMG recording are important variables. High sampling rates, wide enough bandwidth, and flat frequency response [4] are critical for truthful recording of those variables both in EMG and sound analysis.
1.2. Gain
Analog systems for EMG recording, such as Medelec/ TECA, had 9 different gain settings of 50 to 100 000 for amplitude levels from 5 µV to 10 mV. That many settings are not needed for SEMG, but the amplifiers should preferably have a few options for different gain levels. Clipping of amplitudes now occurs freq- uently at strong clenching. The excuse is usually that clipping does not have a significant effect on the integration values. However, analysis of “raw EMG” is also of interest and amplitude is an important vari- able. As an example, the variable kurtosis cannot be calculated correctly if amplitude clipping occurs [5].
1.3. Frequency response and bandwidth
The EMG and sound signals are recorded with two limits for the frequency content, called the high pass (HP) limit and the low pass (LP) limit. The HP limit means that the frequencies lower than that limit are recorded with a lower gain and should not be used in the analysis. The LP limit means that frequencies higher than that limit are recorded with a lower gain and should not be used in the evaluation. Those limits should be set at levels that make it possible to record all frequencies in the signal that may be of interest. They are regarding audible TMJ sounds about 20 Hz to 20,000 Hz and for EMG with needle electrodes 2Hz to 10,000 Hz.
The EMG amplifiers must should preferably have a flat frequency response within the whole frequency area for the signals of interest [6] because to secure that the signal’s different frequencies are amplified with the same gain. The presently used amplifiers have a “hump” in the 100-300 Hz area with decreased gain before and after that bulge.
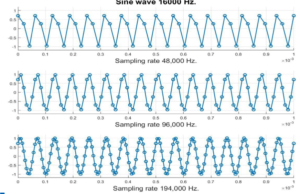
Waveforms are of high interest, the sampling rate should in EMG be at least 10,000 Hz when recording with needle electrodes. The true waveforms of sound waveforms need rates that are up to 200000 Hz which is not a problem with modern sound recording systems. The bandwidth should preferably be adjusted accordingly.
The A/D cards should have as many bits as possible, to get the waveforms closer to what they were in analog recordings.
1.4. Needle electrodes
Recording with intramuscular electrodes used to be a standard part of EMG procedures, also for dentists 50 years ago. Some producers of “SEMG only” tools claim that such an option is not desirable when dentists perform EMG recordings. They motivate this by stating that needle recordings are too painful, too dangerous, and too difficult to be performed by dentists. They could certainly be too painful for some patients 50 to 70 years ago when the EMG needles were much thicker than today’s thin replacements. Pain reaction is, however, not a reason for never using them. Most dentists use needles frequently for injection of anesthetics and some techniques, like the one needed when anesthetizing mandibular molars, is more difficult than most of the techniques for needle EMG recordings from jaw muscles.
There is a risk for hematoma but that is only a real problem when recording from the lateral pterygoid’s upper head. Hematoma is certainly uncomfortable, but the swelling usually disappears after a few days without leaving any permanent damage. The dentist should describe the risks and ask the patient to sign a consent form before making a needle EMG recording. I am not aware of any “hematoma statistics” but will as a comment tell about my own experience during 50 years of clinical practice and 20 years with regular use of needle EMG. I had two cases of hematoma, one when recording from the lateral pterygoid muscle and one from local anesthesia before an upper molar extraction. My own experience is that such a complication is rare.
One situation where the risk for hematoma is not enough important is when a patient suffers from spastic activity and a BOTOX injection is planned. A large part of dental SEMG studies have been about the clinical value of recording higher than normal levels in jaw muscles during mandibular rest. Studies of such activity need to include intramuscular recordings to prove which muscle that is the source of activity [7]. Labeling the activity as coming from a specific muscle without confirmation by needle EMG is only an opinion, not a fact, to paraphrase the famous statement by Dr. Bernard (Barney) Jankelson.
2. MUSCLE BIOMECHANICS
Different parts of the same muscle, such as the deep and superior parts of the temporalis muscle and the deep and the superior parts of the masseter (Figs. 1-4), can have different force vector directions. Nearly identical movements can be created by widely varying muscular forces. Muscles can alternate periods of activity and take turns in activity giving the synergists a pause to rest and thereby minimize fatigue [8]. They may “take turns” in keeping a steady level of force and recording only from one of those can therefore give false information about each muscle’s activity. Decrease of activity may only mean that a synergistic muscle is taking over parts of the work.
Figure 3 is from a frontal section through the medial pterygoid (ep), masseter (m), and lateral pterygoid (lp) muscles. The force vector directions make it possible for the masseter and medial pterygoid muscles to alternate between working as synergists in clenching and as antagonists in mandibular lateral movements. It is also a reminder of how close they are which makes the content of the SEMG recording to be a mixture of masseter and medial pterygoid activity.
Both the masseter and the temporalis have subdivisions that have different force vector directions than other parts of the same muscle. My experience is that SEMG recordings cannot differ between the role of the deep masseter and the superior masseter or between the role of the deep masseter and the deep portion of the temporalis muscle, (Figs. 1-3) when they work as antagonists.
The masseter has about 15 bundles of fibers (Fig. 4) and each bundle can act as a separate muscle. Figs. 1 and 2 illustrate that large parts of the temporalis muscle are deep to the masseter, and that SEMG therefore may be a mixture of temporalis and masseter activity. Note the large mass of the deep temporalis muscle, that is far away from where SEMG electrodes are usually placed for temporalis Surface electrodes placed for recording from the anterior temporalis muscles cannot avoid to also record from the frontal belly of the epicranius that can exert strong activity at frowning and may be activated by pain. They can also pick up activity from the temporo-parietalis or auricularis anterior muscles. A common mistake is to always label SEMG activity during mandibular rest and recorded in the anterior temporalis area as temporalis activity.
3. SOUND CLASSIFICATIONS & UNITS
MSounds are divided into three groups according to audibility for humans, not audible sounds below 20 Hz, audible sounds between 20 Hz and 20,000 Hz, and not audible sounds above 20,000 Hz. Sounds are caused by vibrations, but they are always to be called sounds even if they are recorded after passing only through human tissues, and not through air [9–12].
A very high sampling rate is needed for accurate recording of the sounds’ waveforms. Definition of sounds, adequate labels, and SI units are published by the Physical Society. Academic sources are united in their definitions of sounds, that is, sounds are sounds whether they propagate through air or not before being recorded, whether they are audible or not by the human ear, and sounds are sounds even if nobody was around to hear it [9–12]. Most important when discussing applications in dental clinics is that it does not matter if the sound has travelled through air or not before being recorded.
3.1. Sound recording
Sounds below 20 Hz can be recorded with a Brüel & Kjaer charge accelerometer type 4370 [13] that has a flat frequency response between 0.1 Hz and 4,800 Hz. If sounds under 20 Hz are of interest, the B&K transducer is an excellent choice for recording.
Miniature microphones can be placed in the ear canal close to the sound source. The thickness of the tissues between the source of sounds and the ear canal is only a few mm. In patients with suspected disk displacement with reduction, the difference in loudness between opening and closing clicking is often large. Further studies are required to establish such values, but soundcards with 36 bits A/D conversion are desirable to get as large dynamic range of the patient’s TMJ sound recording as possible.
The amplitude of the recorded sounds depends on the pressure of the transistor against the skin. This varies during the jaw opening due to changes in the condyle position.
3.2. Sound amplifiers 3.2.1. Frequency response and bandwidth
As it is for EMG, a basic request has always been, that sound amplifiers should have a frequency response that is flat. The bandwidth ought to be wide with a low pass cutoff at 20,000 Hz. It would be ideal if the high pass limit was close to zero, but microphones usually have that limit at 20 Hz. If it is important to also detect sounds with frequencies below 20 Hz, the recordings must be complemented with soundtracks made with special sensors that can record such frequencies.
3.2.2. Sampling rate
Figure 4 shows how increasing the sampling rate from 48,000 Hz to 194,000 Hz improves the quality of the recorded waveform of a 16,000 Hz sineway. Each small circle marks the position in the sinewave. With a sampling rate of 48,000 Hz about 4, and with 194,000 Hz about 12-13 positions are marked in each single sinewave.
Figure 5 has a contour plot in the left window of a TMJ clicking sound and the original waveform of the clicking is shown in the right window. It was recorded with a miniature microphone placed in the ear canal. The colors represent energy levels on a scale from low (blue) to high (yellow). The plot shows that the area with energy is at about 5000 Hz to 6000 Hz, which also is the area with highest audibility for the human ear.
3.3. Artifacts in sound recording
Skin contact transducers, such as those used in JVR recordings [15], can also record movements, that cause artifacts in the sound recording [16]. They are especially sensitive to sudden jerky condylar and cable movements.
3.4. Wave forms
Graphs of TMJ sounds’ waveforms can be misleading if the sampling rate is too low. Because very few studies have been made with high quality miniature microphones, we still do not know what the LP limit is, but we do know that it is at least about 16,000 Hz. The sampling rate of 194,000 Hz is needed for high quality recordings of the forms of the highest audible frequencies (Fig. 6). The size of such data records was too large for old time computers, but they are not for today’s versions. Modern amplifiers for sound recording, have a bandwidth of about 20 Hz to 20,000 Hz.
3.5. Time constant – the forgotten factor
Recording of TMJ sounds, combined with jaw movement recording, is a valuable tool in diagnosis and analysis of the relations between TMJ sounds and disk position [16,17]. The time location during jaw movements of clicking is a helpful information. The time constant for sounds is less than a millisecond (ms) [18]. However, for jaw movement recordings, it can be as large as 40 ms [21] which can be a significant error because a fast jaw opening-closing movement can take less than 100 ms. [19]. If looking for the causes of TMJ clicking, it is needed to also record during fast and not only during slow movements. A problem is that the exact values of time constants are seldom, if ever, reported in the relevant equipment manuals.
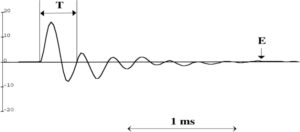
3.6. Possible harmful effect on hearing ability of TMJ sounds
Clicking is often a snapping sound (Fig. 7) and the peak loudness may last only for about 0.2 ms. The amount of energy can be very low even if the dB level is high. That can explain why clicking with high dB levels may not cause immediate damage. Clinical experience tells us that some patients can have clicks, that can be heard several meters away. It is therefore possible that TMJ clicking as heard by the patient himself can have levels well above the 85 dB, that is the common limit for potentially harmful sounds. It should be noted, however, that dB is not a loudness variable Audible sounds can have very high dB levels while the loudness is low. The possible longtime effects of chronic audible clicking should not be ignored and deserve more attention in research. Fig. 7 shows the wave form of a typical short duration clicking (snapping) sound. Note the exponential decay of amplitude down to noise level (arrow E) after about 2 ms. Some patients have clicking that can be heard 6-8 m away. A question of interest is, how high would the loudness level be as heard by the patient with such clicking, and can it be harmful? This could be researched by comparing hearing ability between sides in subjects with chronic unilateral TMJ sounds. The dB level of strong clicking may be about 130 dB but still not harmful, if the time duration is short, a few ms. or less. Future studies are needed.
4. FLOW CHARTS
Models have been designed to help in diagnosis. They are often designed as flow charts [23] but without the probability of the answers to each step being correct. That may often be lower than 80 %, but even if it is that high, it takes only a few steps before the probability of correct guidance is about 50 % or less. If the probability of the correct answer to each step is 80 %, the credibility of the answer to a step will be 80% of the probability of the preceding step. In a flow chart with 4 steps the probability will be 1st step 80%, 2nd step 64%, 3rd step 51 %, and 4th step 40.8 %. This means that it would be deceptive to have more than two steps in a flow-chart.
5.CONCLUSION
The following options in equipments used for EMG recordings in dental clinics are suggested to be standard. Options for intramuscular electrodes and microphone input.
Options for multiple gain settings to avoid clipping of amplitudes.
Options for increased bandwidth for EMG to 2Hz – 10,000 Hz, and sounds to 20 Hz – 20,000 Hz,
Flat frequency response in amplifiers to make sure that all recordable frequencies are documented with the same gain.
SEMG of masseter and temporalis activity can be a source of misconceptions regarding the role of parts with different force vector directions such as between the deep and superior parts of the masseter and between the zygomatico-mandibular and the deep temporalis muscle. The value of integration of EMG as a method can be discussed but classical methods for analysis of “raw EMG”, that is not integrated EMG, should not be abandoned. It is motivated to update the presently used equipment in a way that true amplitude values, waveforms, EMG pattern, can be recorded within the full bandwidth of the signals without clipping or distortion of form.
The TMJ sounds are called sounds even if they are in not audible frequency areas and whether they have passed through air or not.
Flow-charts should consider the probability of the statements or questions in each step.
Widmalm SE. The need for improved standards of commonly used equipment for recording of EMG and TMJ sounds in dental clinics. Stoma Edu J. 2023;10(1-4):13-18.
CONFLICT OF INTEREST
Author declare that there is no conflict of interests.
References
- Tursky B. Integrators as measuring devices of bioelectric output. Clin Pharmacol Ther. 1964;5(6part2):887-892.
Google Scholar
- Basmajian JV, de Luca CJ. Muscles alive: their functions relieved by electromyography. 5th ed. Baltimore, MD: Williams & Wilkins; 1985.
- Grossman WI, Weiner H. Some factors affecting the reliability of surface electromyography. Psychosom Med. 1966 Jan-Feb;28(1):78-83.
Google Scholar Scopus
- Stålberg E, Trontelj JV. Single fibre electromyography. Surrey, UK: The Mirvalle Press Ltd.; 1979.
- Dong Y, Li B, Hu J, Widmalm SE, Zhang T, Lin M, Buvarp A, Zhou D. Kurtosis, a new variable with possible diagnostic value in analysis of jaw muscle surface EMG. J Oral Rehabil. 2022 Feb;49(2):170-176.
Full text links CrossRef PubMed Google Scholar Scopus WoS
- Williams WJ. Biological applications and interpretations of time-frequency signal analysis. In: Akay M, Ed. Time frequency and wavelets in biomedical signal processing. New York, NY:
Wiley-IEEE Press; 1997. pp 45-72.
Google Scholar
- Hu J, Dong Y, Widmalm SE, Buvarp A, Zhang T, Li B, Lin M, Zhou D. Is SEMG recorded “hyperactivity” during mandibular rest a sign of dysfunctional jaw muscle activity and temporomandibular disorders (TMD)? J Oral Rehabil. 2020 Aug;47(8):930-938.
Full text links CrossRef PubMed Google Scholar WoS
- Knudson D. Fundamental of Biomechanics. Springer Science + Business Media LL.; 2007.
Google Scholar
- Norton MP. Fundamentals of noise and vibration analysis for engineers. Cambridge, UK: Cambridge University Press;1989. p106.
Google Scholar
- Kinsler LE, Frey AR, Coppens AB, Sanders JV. Fundamentals of acoustics. 4th ed. New York, NY: John Wiley & Sons; 2000.
Google Scholar
- College Physics. Houston, TX: Rice University; 2020. Available from: https://openstax.org/details/books/college-physics.
- Beranek LL. Acoustics. Woodbury, NY: the Acoustical Society of America; 1996.
Google Scholar
- Widmalm SE, Bae HE, Djurdjanovic D, McKay DC. Inaudible temporomandibular joint vibrations. Cranio. 2006 Jul;24(3): 207-212.
Google Scholar
- Widmalm SE, Williams WJ, Djurdjanovic D, McKay DC. The frequency range of TMJ sounds. J Oral Rehabil. 2003 Apr;30(4):335-346.
Full text links CrossRef PubMed Google Scholar
- Radke JC, Velasco GR. JVA measurements of TMJ function. In: The Diagnostic Value of Biometric Instruments. San Antonio, TX 78254: An Open eBook from Advanced Dental Technologies & Techniques; 2021. p 7.
- Widmalm SE, Dong Y, Li BX, Lin M, Fan LJ, Deng SM. Unbalanced lateral mandibular deviation associated with TMJ sound as a sign in TMJ disc dysfunction diagnosis. J Oral Rehabil. 2016 Dec;43(12):911-920.
Full text links CrossRef PubMed Google Scholar Scopus WoS
- Isberg-Holm AM, Westesson PL. Movement of disc and condyle in temporomandibular joints with and without clicking. A high-speed cinematographic and dissection study on autopsy specimens. Acta Odontol Scand. 1982;40(3):165-177.
Full text links PubMed Google Scholar Scopus
- Westesson P. Diagnostic imaging of internal derangements of the temporomandibular joint. Current Controversies in Surgery of the Temporomandibular Joint. Oral Maxillofac Surg Clin North Am. 1994;6(2):227-244.
- Widmalm SE, Hedegard B. Reflex activity in the masseter muscle of young individuals. I. Experimental procedure – results. J Oral Rehabil. 1976 Jan;3(1):41-55.
Full text links CrossRef PubMed Google Scholar Scopus
- Widmalm SE. Tooth tapping ability of young and elderly males and females. J Oral Rehabil. 1977 Apr;4(2):169-180.
Full text links PubMed Google Scholar Scopus WoS
- Widmalm SE, Larsson EM. A new method for recording temporomandibular joint sounds and electrical jaw muscle activity in relation to jaw opening degree. Acta Odontol Scand. 1982;40(6):429-434.
Full text links CrossRef PubMed Google Scholar Scopus WoS
- Widmalm SE, Williams WJ, Adams BS. The wave forms of temporomandibular joint sound clicking and crepitation. J Oral Rehabil. 1996 Jan;23(1):44-49.
Full text links CrossRef PubMed Google Scholar Scopus WoS - Radke JC, Velasco GR. JVA measurements of TMJ function. In: The Diagnostic Value of Biometric Instruments. San Antonio, TX 78254: An Open eBook from Advanced Dental Technologies & Techniques; 2021. Chapter 1. p 13.
- Schumacher GH. Funktionelle Morphologie der Kaumuskulatur. Jena: Gustav Fischer Verlag; 1961, p 1-53.
Google Scholar
DDS, PhD, Professor Emeritus Computer Science and Engineering Division College of Engineering University of Michigan Ann Arbor, MI 48109, USA
CV
Sven Erik Widmalm (DDS) is Specialist of Stomatognathic Physiology certified by the Swedish National Board of Health and Welfare, Professor Emeritus, University of Michigan, Scientific Research Consultant at the Second Affiliated Hospital Zhejiang University School of Medicine.
Widmalm worked as Senior Researcher at the Karolinska Institute, Stockholm, and later at the University of Michigan, School of Dentistry, and as Adjunct Research Scientist, at the Electrical Engineering & Computer Science College of Engineering University of Michigan.
Widmalm has been a Visiting Professor, at Yonsei University, Seoul, Korea, at Chosun University, Guang-ju, Korea, at Fourth Military Medical University, Xi’an, Shaanxi Province, China, and at Zhejiang University.
Widmalm’s doctoral thesis was based on electromyographic (EMG) recordings of jaw reflex activity. He has published original research based on anatomical dissections, TMJ sound, and electromyographic jaw muscle studies.
Questions
- What should the gain of a surface EMG amplifier be?
- The gain should be 1000;
- The amplifier should have options for different gain settings at low and at high activity. They should be variable from high to differ between rest and low activity to high enough to avoid clipping at maximal activity;
- The gain should be 5000;
- The gain should be 10,000.
- How should the frequency response be for a TMJ sound/vibration amplifier?
- The frequency response should be limited to frequencies below 1000 Hz and higher for a specific area, such as 100Hz to 300 Hz than for the other areas;
- It can be “curved” and a flat frequency response is not needed;
- The amplifier should ideally have a flat frequency response for audible sounds/vibrations (20 Hz to 20,000 Hz);
- The amplifier should record the frequencies below about 500 Hz.
- What type of sensor or technique is best for TMJ sound/vibration recording?
- Skin contact transducer;
- Miniature microphones;
- Stethoscope;
- Finger palpation.
- TMJ sound analysis:
- Vibrations cannot be called sounds unless they pass through the air before being recorded;
- Sounds above 1000 Hz are not of clinical interest;
- Not audible vibrations cannot be called sounds;
- Sounds are called sounds even if they do not pass through the air before being recorded.
Figure 1 A head section in a frontal plane behind the eye bulbs and the molar teeth.The main parts of the temporalis (t), masseter (m), tongue, and the mylohyoid muscles under the tongue are seen.

Figure 2 Close-up of a temporalis masseter section. The deep portion of the temporalis muscle (1) with origin in the lowest part of fossa temporalis and inserting in the medial side of processus coronoideus (5), has an antagonist in the deep portion of the masseter muscle (3), also called the zygomatico-mandibular muscle. The superior part of the masseter (2). The mandibular body (4).The part immediately behind the eye (6).The tongue (7). The nasal cavities (8). The adipose tissue between the skin and the muscles (9).
Figure 3 A frontal section through the medial pterygoid (ep), masseter (m), and lateral pterygoid (lp) muscles. The deep masseter is seen in the upperrightcornerwithoriginatthedistalsideoftheprocessuscoronoideus and an insertion into arcus zygomaticus.
Figure 4 This figure from reference 24 illustrates the differences in orientation of muscle bundle subdivisions of the superior and the deep masseter. Both have separate fiber bundles with individual directions of the force vectors. Presently biomechanical SEMG studies are based on the false assumption that the jaw muscles always has only one force vector direction. This is true about many arm and leg muscles. The masseter and the temporalis have however parts with significantly different force vector directions. In the study of jaw muscle biomechanics, SEMG can be misleading because the directions of force vectors can differ significantly between superficial and deep parts depending on which bundles that are active.
Figure 5 This figure is a contour plot of a TMJ clicking sound recorded with a miniature microphone.The colors represent energy levels on a scale from low (dark blue) to high (red).The plot shows that the bandwidth of the sound is about 100 Hz to 12,000 Hz, with the energy peak at about 6,000 Hz. The colors represent energy levels on a scale from low (dark blue) to high (red).
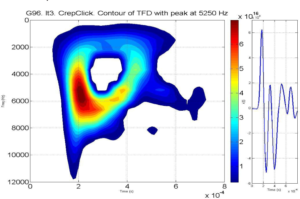
Figure 6 The small circles on the waveform mark the position of each consecutivesampleoftherecordedsineway.Anacceptablerepresentation of the waveform was obtained when the sampling rate was 196,000 Hz. This is no problem if modern amplifiers are used.
Figure 7 The wave form of a short duration clicking (snapping) sound. Noise level (arrow E) is reached after about 2 ms. T = temporal period duration. Amplitude level is in arbitrary units.